Uterine Health: The Need for Better Solutions
Uterine conditions affect women across every stage of life, yet diagnosis and treatment remain fragmented and often invasive.
Fibroids are benign growths that develop in the uterine muscle and affect up to 70% of women by age 50, and more than 80% of Black women [3].
Adenomyosis, another major cause of pain and heavy menstrual bleeding, occurs when the tissue that normally lines the uterus (the endometrium) grows into the muscular wall of the uterus (the myometrium). Each month this tissue thickens and bleeds inside the muscle layer, causing inflammation, swelling, and pain. The uterus can become enlarged and tender, and many women report severe cramping, heavy periods, or pelvic pressure. Unlike fibroids, which form discrete growths, adenomyosis spreads throughout the uterine wall and may coexist with fibroids or endometriosis. It is often under-recognized because imaging criteria vary and symptoms overlap with other conditions [4,5,6,7].
Endometrial cancer is the most common gynecologic cancer in the United States, yet there is currently no standard screening test. Most cases are detected only after women experience abnormal bleeding, and diagnosis requires invasive procedures like endometrial biopsy or dilation and curettage (D&C). The lack of proactive screening, plus no standard for what's "normal" bleeding vs "heavy" bleeding, means many women face delays in diagnosis. Early detection is critical, as survival rates remain high when cancer is confined to the uterus but drop significantly once it spreads.
Because these conditions share overlapping symptoms, heavy or prolonged bleeding, pelvic pain, infertility, they require coordinated care and specialized diagnostic tools. Several technologies now aim to quantify menstrual bleeding, using digital tools and connected products that can help women track changes and start informed conversations with clinicians who can then order appropriate screening or diagnostic tests [8].
Trends Shaping Uterine Health Innovation
Innovation in uterine health is accelerating through digital and software-based approaches that connect symptom tracking, imaging, and treatment outcomes.
- Digital bleeding quantification: Mobile apps, connected devices, and smart menstrual products are transforming subjective symptom tracking into measurable data, allowing better evaluation of heavy menstrual bleeding and treatment effectiveness [9].
- Software as a Medical Device (SaMD): Predictive algorithms and AI models are emerging to support early recognition of abnormal bleeding and fibroid risk while maintaining clinical oversight and regulatory compliance.
- AI-enhanced imaging: Ultrasound and MRI software now use machine learning to identify fibroids, adenomyosis, and endometrial abnormalities with greater accuracy.
- Interoperability and integration: Data pipelines connecting menstrual apps, lab platforms, imaging systems, and clinician dashboards are shaping the foundation of connected uterine care.
- Virtual care and remote monitoring: Telehealth and software-driven follow-up tools allow ongoing symptom monitoring after procedures or interventions.
- Equity and inclusion: New digital tools and datasets are focusing on historically underrepresented populations, addressing racial disparities in uterine conditions and treatment outcomes.
Evidence of Acceleration: Clinical Trials and Patent Activity
Clinical Trials
Recent studies show a growing focus on digital and software endpoints in uterine care.
- The Apple Women's Health Study is collecting large-scale digital data on menstrual cycles, bleeding patterns, and symptom tracking, creating new research baselines for uterine health [10].
- Randomized trials are validating digital symptom tracking and bleeding quantification tools as part of heavy menstrual bleeding research [11,12,13].
- AI and imaging-based trials are exploring automated detection of uterine lesions laying groundwork for future SaMD solutions.
Patent Activity
Patent filings highlight rapid innovation in:
- AI-assisted imaging for uterine and endometrial pathology detection
- Digital blood-loss estimation and menstrual tracking algorithms
- Software modules that integrate patient-reported outcomes, imaging data, and clinical alerts
- Connected dashboards for remote post-procedure monitoring
These trends point to a clear shift toward software-driven diagnostics and digitally supported clinical workflows.
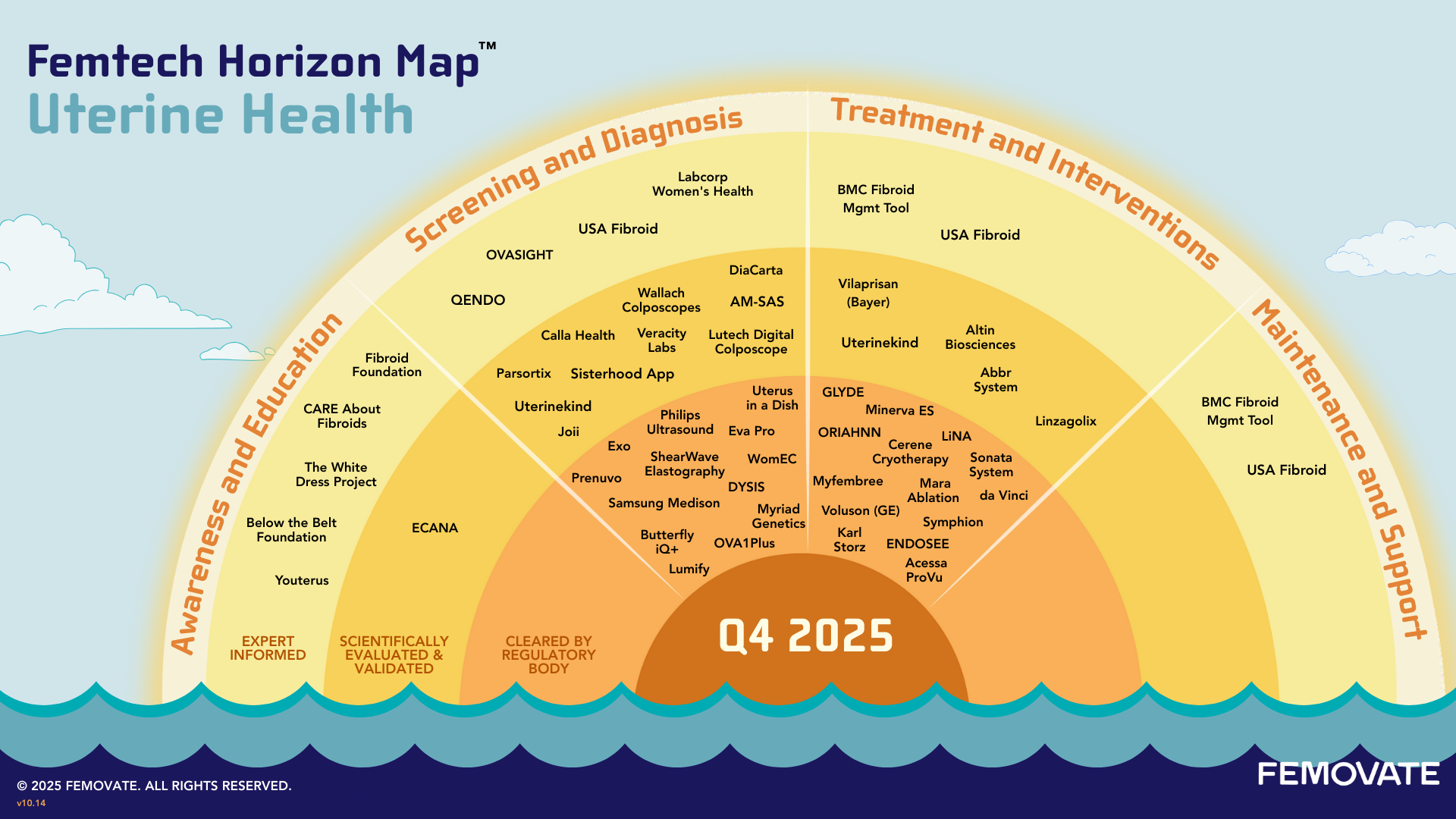
These trends come to life through the companies and technologies we’ve mapped across the continuum of care. The examples below highlight where innovation is gaining traction and where significant gaps remain.
Emerging Technologies Across the Continuum of Care
Awareness & Education
Digital communities and education platforms are expanding access to reliable information and helping women recognize abnormal symptoms sooner. Organizations including The Fibroid Foundation, CARE About Fibroids, The White Dress Project, and The Endometrial Cancer Action Network for African-Americans (ECANA) provide expert-informed content, advocacy, and community support. These platforms help normalize conversations about uterine health and reduce barriers to seeking care.
Screening & Diagnosis
This stage of the continuum is seeing rapid innovation across multiple fronts:
- AI-enhanced imaging: Portable and AI-powered ultrasound devices from companies like Butterfly Network, Exo, and Samsung Medison are bringing advanced imaging capabilities to more care settings. These tools use machine learning to improve detection of fibroids and adenomyosis, while advanced systems like Hologic's ShearWave™ Elastography add tissue characterization capabilities.
- Digital colposcopy: Companies such as DYSIS Medical, MobileODT, and Calla Health are advancing cervical and uterine visualization with digital colposcopy systems that use AI and smartphone integration to improve detection accuracy and accessibility.
- Cancer screening and early detection: Unlike cervical cancer, which has established screening protocols, endometrial cancer has no routine screening method. Biomarker tests such as MiMARK's WomEC represent an important advancement, offering non-invasive detection that could identify cancer earlier than the current standard of waiting for symptoms. Myriad Genetics and Angle PLC's Parsortix system are also expanding early cancer risk and surveillance capabilities.
- Biomarker and lab innovation: At-home testing from companies such as Veracity Labs expands access to hormone and metabolic screening that can identify risk factors for uterine conditions.
- Emerging diagnostic tools: Innovations such as Joii's diagnostic tampon for menstrual fluids create new, less invasive methods for tissue sampling and biomarker collection.
- Digital bleeding quantification: Products in this category enable women to capture objective data that supports clinical decision-making, an important step between symptoms being raised and formal diagnosis.
Treatment & Interventions
The treatment landscape spans minimally invasive surgical systems, energy-based therapies, and pharmaceutical interventions.
- Minimally invasive surgery: Robotic-assisted platforms like Intuitive Surgical's da Vinci system and hysteroscopy equipment from Karl Storz and CooperSurgical are enabling more precise, less invasive procedures for fibroid removal and endometrial treatment.
- Energy-based therapies: FDA-approved systems such as Gynesonics' Sonata, Minerva Surgical's Minerva ES, Aegea Medical's Mara, and Nesa Medtech's GLYDE offer alternatives to traditional surgery. Nesa Medtech is also advancing its Abbr™ focused ultrasound system through clinical trials.
- Pharmaceutical interventions: FDA-approved therapies including AbbVie's ORIAHNN and Myovant Sciences' Myfembree have expanded non-surgical options for managing fibroid symptoms. Additional therapies from ObsEva, Bayer, and Altin Biosciences are progressing through clinical development.
- Innovative platforms: Opal Therapeutics' “Uterus in a Dish” technology represents a new way to study disease mechanisms and test treatments, bridging research and clinical application.
Procedure-planning software and intraoperative navigation tools are enhancing precision across these interventions, while remote care platforms are emerging for post-procedure tracking and recurrence monitoring.
Maintenance & Support
There is growing demand for longitudinal views that combine period data, imaging, and hormone tracking, allowing ongoing care and feedback loops between patients and clinicians. This remains one of the largest gaps in uterine care, as you can see in the map, with few established tools for monitoring after treatment and interventions.
Where Gaps Remain
Despite the acceleration in uterine health innovation, several areas remain underserved:
- No routine screening for endometrial cancer.
- No standard way for women and their providers to align on what's "normal" vs "heavy" periods.
- Fragmented data across apps, imaging, labs, and patient records.
- Limited options for post-treatment managing and monitoring, generic post surgical support systems exist, but very few uterine health optimized offerings.
- Underinvestment in adenomyosis-specific solutions.
- Racial disparities in outcomes persist, with few innovations explicitly addressing the screening, diagnostic, and treatment gaps that contribute to these disparities.
Market Outlook and Emerging Signals
Several signals point to rapid progress in digital and software-enabled innovation for uterine health.
- Regulatory activity: The FDA Digital Health Center of Excellence and comparable EU bodies are reviewing submissions for software that quantifies menstrual blood loss, interprets imaging data, or supports diagnostic pathways for abnormal bleeding and fibroids.
- Clinical validation: Trials on ClinicalTrials.gov increasingly include digital endpoints such as app-based bleeding logs, remote symptom monitoring, and AI-assisted imaging analysis.
- Industry partnerships: Imaging and diagnostics companies are collaborating with digital health startups to embed algorithms, share datasets, and extend device value through connected software.
- Payer and employer pilots: Health plans and employer benefits programs are testing whether digital monitoring and early detection can lower the cost and frequency of high-expense procedures.
- Investment momentum: Investors are funding hybrid platforms that combine bleeding quantification, AI-guided imaging, and virtual care coordination. These efforts are building the foundation for integrated uterine care ecosystems.
Together, these signals suggest that the next phase of uterine innovation will be led by data-driven, software-first solutions. The focus is shifting from new drugs or hardware toward connected digital frameworks that link detection, diagnosis, and long-term management in one continuous care experience.
What’s Needed Now
The uterine health landscape needs continued investment and development in key areas:
- Validated cancer screening tools that can identify endometrial cancer before symptoms appear.
- Clinical-grade validation and regulatory clearance for digital bleeding quantification tools.
- Integration platforms that connect patient-reported data, imaging, lab results, and clinical workflows.
- Longitudinal care models that support women through treatment and into maintenance, with tools to monitor recurrence and treatment effectiveness.
- Equity-centered design that addresses the disproportionate burden of uterine conditions on Black women and other underserved populations.
- Partnerships that bring together diagnostics, digital health, providers, and payers to create coordinated care ecosystems.
The Femtech Horizon Map for Uterine Health is a starting point for identifying these opportunities and accelerating meaningful progress in women’s health.
Sources
- Cardozo, E. R., et al. "The estimated annual cost of uterine leiomyomata in the United States." American Journal of Obstetrics and Gynecology, 2012.
- Soliman, A. M., et al. "The direct and indirect costs of uterine fibroid tumors: a systematic review of the literature between 2000 and 2013." Journal of Women's Health, 2017.
- Baird, D. D., et al. "High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence." American Journal of Obstetrics and Gynecology, 2003.
- Levgur, M., et al. "Adenomyosis: symptoms, histology, and pregnancy terminations." Human Reproduction Update, 2000.
- Abbott, J. A., et al. "Adenomyosis: a clinical review." Fertility and Sterility, 2003.
- Dueholm, M., et al. "Ultrasound imaging techniques in the evaluation of pelvic pain." Ultrasound in Obstetrics & Gynecology, 2018.
- Mayo Clinic. "Adenomyosis." 2024.
- Wyatt, K. M., et al. "Menstrual blood loss measured using a pictorial assessment chart." BJOG: An International Journal of Obstetrics & Gynaecology, 2001.
- "Digital tools for menstrual bleeding assessment." BMC Women's Health, 2023.
- Apple Women's Health Study. "Large-scale study of menstrual cycles and gynecologic conditions." PMCID: PMC9877138.
- Fortin, C. N., et al. "Mobile Application vs Paper Pictorial Blood Assessment Chart to Track Menses in Young Women: A Randomized Cross-over Design." Journal of Pediatric and Adolescent Gynecology, 2018.
- Samuelson Bannow, B. T., et al. "Comparison of Paper Diaries, Text Messages and Smartphone App to Track Bleeding and Other Symptoms for Contraceptive Studies." Contraception, 2022.
- Lee, J., & Kim, J. "Can menstrual health apps selected based on users' needs change health-related factors? A double-blind randomized controlled trial." Journal of the American Medical Informatics Association, 2019.
Leverage Our Expertise
Femovate is a women-owned, women-led company specializing in product strategy, design, and validation for women's health solutions. When you're developing a product, platform, or new business concept, our team can help bring your innovation to market.
About Femtech Horizon Maps
Our Femtech Horizon Maps highlight the latest technologies across women's health, showing where innovation is emerging and what gaps remain to be filled. By visualizing the entire continuum of care for specific verticals, we aim to inspire the development of integrated platforms that support women throughout their healthcare journeys. These maps help industry stakeholders find opportunities, address gaps, and develop more effective solutions.
Partner With Us on the Maps
Are you a clinical expert, innovator, or passionate advocate for women's health? Help us on our next maps: breast health and hormonal health, just send us a message through LinkedIn. If you have feedback on this map, please reach out.