At any given time, more than 25% of the world’s population is menstruating. Menstruation shapes health, education, and economic participation worldwide, yet menstrual disorders such as irregular cycles, heavy bleeding, and extreme pain remain underdiagnosed and widely dismissed. These disorders drive absenteeism and – more commonly – presenteeism, which lowers productivity and has a significant economic impact.
One recent study found that menstrual symptoms account for the equivalent of nine lost productivity days per person each year, with more than eighty percent of the economic impact due to reduced performance at work rather than absence. A large Dutch study found that menstrual symptoms cost an estimated €1.9 billion nationwide each year, most of that from women working through pain and feeling unwell rather than staying home.¹ ²
In low‑resource settings, severe pain and heavy bleeding correlate with lower academic performance, reduced sports participation, and higher dropout risk. One in three female students regularly misses school because of menstrual symptoms or a lack of supplies, a pattern documented across multiple regions.³
Despite such measurable impacts, menstrual symptoms are rarely treated as clinical vital signs. Many women navigate symptoms alone for years before receiving evaluation or appropriate care. Where healthcare systems have lagged, we are beginning to see technological advances aiming to focus on menstrual health issues.
In researching this report, we found that menstrual health also sits at the intersection of other femtech frontiers. Our companion article and map, Monthly Intelligence: The Rise of Menstrual Diagnostics, explores menstrual effluent as an exciting diagnostic frontier. For endometriosis‑specific innovation, our Femtech Horizon Map for Endometriosis covers tools for diagnosis, treatment, and long‑term management of one of the most common causes of debilitating menstrual pain.
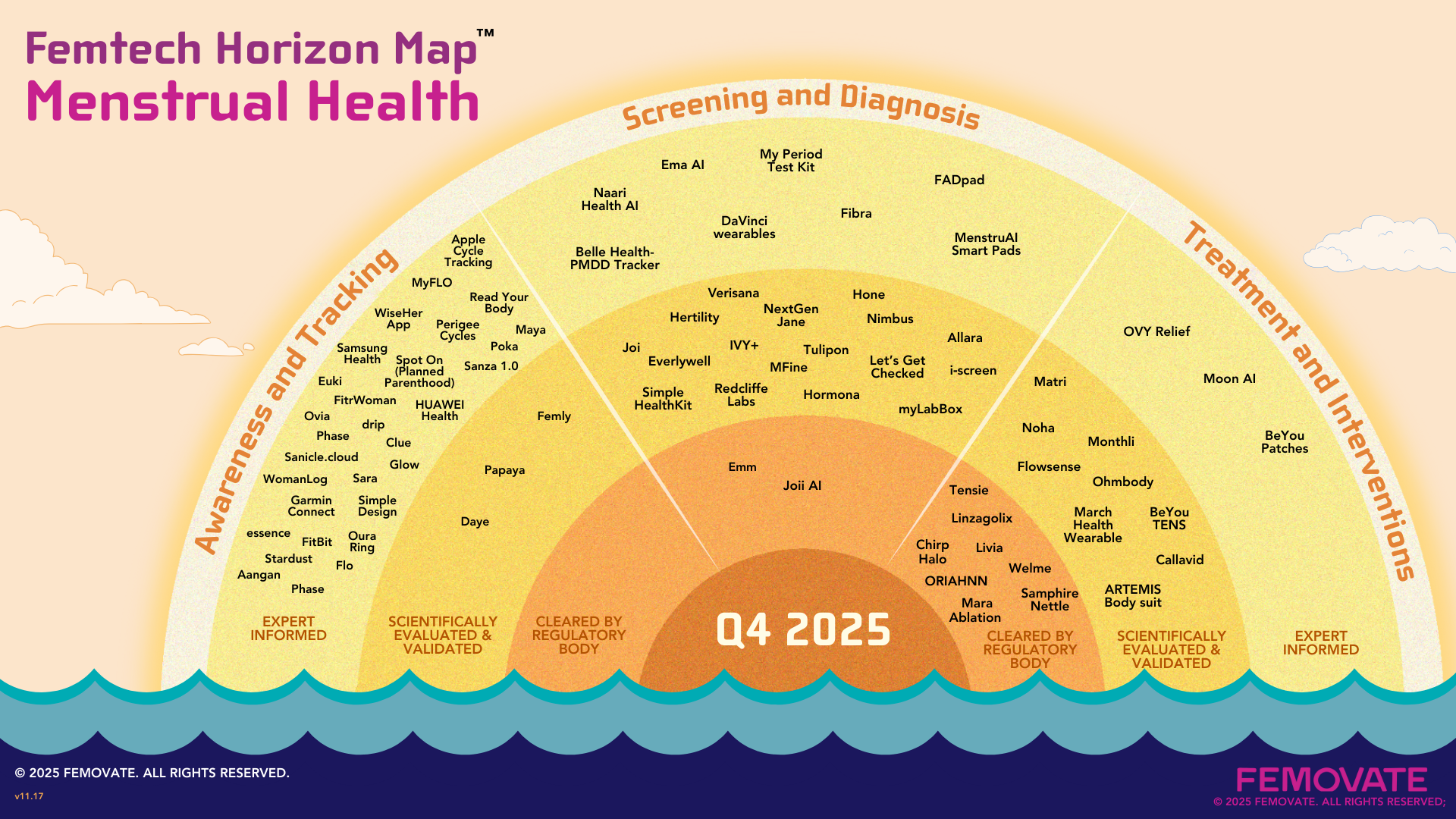
Looking at the Horizon Map for Menstrual Health, it’s clear that innovation is accelerating across the continuum of care, but progress is uneven; some areas have reached global scale, while others remain early or fragmented. The landscape also appears to be shifting from high-level awareness toward deeper clinical understanding and relevance. For this map, we looked at three phases of clinical need:
The number of high-quality, insightful cycle tracking apps has exploded. Here’s what we found:
Awareness & Tracking apps are at global saturation
Awareness tools are the most mature part of the menstrual health landscape. Our map shows only a fraction of the global cycle‑tracking apps available today, and more are being launched every day. This saturation represents genuine progress: millions of women now have access to cycle education, tracking, and symptom literacy that did not exist a decade ago.
Cycle data is powerful, but it is not yet integrated fully in healthcare
Cycle and symptom tracking apps are a good step forward, but so far this awareness has not translated to clinical practice. Nearly all of this data remains trapped in consumer app silos, unable to connect with electronic health records (EHRs), clinical decision tools, or research datasets. If a patient wants to share this valuable information with their doctor, they typically bring screenshots or limited summary exports to clinical visits. Because this data is unstructured and can’t integrate with clinical symptoms, healthcare providers may not recognize its value. A small number of platforms are beginning to explore clinically relevant data‑sharing pathways that could support screening, referrals, and early intervention. The Apple Women’s Health Study creates structured cycle logs, and Oura offers CSV downloads and clear PDF summaries designed to help users communicate insights, questions, and concerns with their doctors more effectively. While this type of reporting is not true EHR integration, it signals a positive step in that direction. The bottom line: Millions of patients understand their cycles better than ever, yet healthcare systems have not adapted to use this information. Clinical integration is complicated, but the opportunity is huge for companies willing to take on the challenge.
Serious privacy concerns
Privacy and data security remain inconsistent across cycle‑tracking tools, and users are becoming more wary about logging sensitive information after several companies were fined for sharing sensitive data with third parties. Flo, for example, reached a settlement after sharing users’ cycle information with Meta for advertising purposes, highlighting how easily menstrual data can be misused without explicit safeguards. Oura recently dealt with fallout from a social media rumor that turned out to be false. The company was able to show transparency and quell the disinformation, however the incident raised patient concerns about what tracking apps can do with their private health information. Other apps such as Comma and Clue differentiate themselves through clear, ethical data‑handling practices, and plenty of opportunities exist for companies that reassure customers on this front. For now, users must pay close attention and educate themselves before clicking “Agree.”
Historically, women have faced barriers to diagnosis, as clinicians disagreed about the definition of normal vs abnormal menstrual cycles. We are excited to see signs that diagnostic technology and research will not only validate patient concerns, but will help identify abnormalities much earlier. The Horizon Map includes digital screeners for heavy menstrual bleeding, smart pads and underwear that estimate blood loss, and at‑home sampling devices supporting crucial biomarker analysis. We see that the evidence supporting these innovations ranges from early expert‑informed tools to regulatory pathways for bleeding assessment that promise to shift menstrual health from subjective descriptors toward objective, quantifiable clinical signals.
We also found some interesting evidence of acceleration in IP and research:
Together, these signals suggest that menstrual health is moving from under‑explored to actively engineered, with more tools being designed, tested, and protected each year.
Given the barriers that women face when seeking clinical care for menstrual pain and heavy bleeding, it is not surprising that there’s a high demand for direct-to-consumer interventions. Classified on our map as Expert-informed solutions, this area includes digital pain relief tools using heat, vibration, or sound in a way that is discreet and easy to use. Femtech Horizon Maps focus on technological solutions, but it is worth noting that we also found a wide array of over-the-counter topical products, CBD formulations, and other non-tech offerings.
In the middle tier of the map, Scientifically evaluated & validated interventions section, we can see that companies are testing novel ways to measure and relieve pain. At the highest‑evidence Cleared tier, neuromodulation and TENS‑based devices now have regulatory clearance for menstrual pain relief, and minimally invasive technologies are emerging to reduce heavy bleeding.
Overall, the trend within treatment and interventions is clear: solutions are becoming more user‑controlled, more portable, and easier to integrate into daily life. They do not replace the need for improved diagnostics, but they help address the immediate needs of millions of women and girls experiencing menstrual pain.
Menstrual health must move toward a more connected and clinically relevant future. The next phase of innovation calls for better continuity across the full care experience: linking awareness to earlier diagnosis, connecting screening outputs to clinical systems, and ensuring that scientifically validated treatments become widely available.
Positive trends that require ongoing funding and support
Where Gaps Remain
Advancing menstrual health will require a coordinated system that connects the tools women already use with the clinical pathways they need. Three themes emerged clearly across this landscape:
Achieving this vision will require strategic partnerships between consumer apps, big tech, medtech innovators, researchers, and healthcare organizations. These collaborations are needed to define new standards of care and ensure that insights generated at the awareness stage flow into screening, diagnosis, and evidence‑based treatment pathways. Women should not have to self‑triage between consumer wellness products and medical care. We hope to eventually see a more unified ecosystem where menstrual health is finally treated as a meaningful part of whole-person health, rather than an isolated monthly experience.
Our Femtech Horizon Maps highlight technologies across women's health, showing where innovation is emerging and where gaps remain. By visualizing entire care landscapes, these maps help founders, clinicians, and investors identify opportunities, address unmet needs, and build more integrated solutions. This is the 5th map in our series of 20 maps across all women's health verticals.
Femovate is a women‑owned, women‑led company specializing in product strategy, design, and validation for women's health solutions. If you are innovating in women's health, our team can support commercialization strategy, product research, design and implementation to help you launch and scale your solution.